Blog

November 06, 2025
Essential oils promote Neuroplasticity Confirmed – a groundbreaking study on essential oils and gray matter volume
Thank you so much to Kathy Drury for bringing this study to my attention.
For years, I have passionately promoted the concept that essential oils possess the power to enhance neuroplasticity—the br...
Read More

Book Reviews
July 28, 2025
A profound gaze into the soul of aging: a review of the novel 'The Elderly'
A book by Paula De Sousa Lima, translated by Dinez Borges, English edition published by Bruma Publications.
For a long time, I've wanted to share my thoughts on a truly exceptional book, but it t...
Read More

perfume
July 27, 2025
Would you buy a perfume without ever having smelt it?
I came across an insightful article in CosmeticsDesign Europe titled “What makes someone buy a perfume they have never smelled before?” by Sarah Cohen, published on 17 July 2025.
Sarah Cohen, the a...
Read More
July 08, 2025
Book Review: The Smell of Fresh Rain by Barney Shaw
I want to share with you one of my all-time favourite books on scent, first published in in 2017, by Barney Shaw. The title of the book – The Smell of Fresh Rain is so inviting and evocative. It gi...
Read More

May 28, 2025
In memory of Jonathon Benavides
Sometimes, when tragedy strikes, I find myself at a loss for words, retreating inward with my grief. This was certainly the case when I heard about the passing of Jonathan Benavides. The news came ...
Read More
Book Reviews
February 12, 2025
Book Review - Historical Perspectives on Smell by Jonathan Reinarz
The book's strength lies in its meticulous research and its ability to weave together diverse strands of historical inquiry, including social history, medical history, cultural studies, and even li...
Read More
Book Reviews
January 09, 2025
Book Review - Magical Aromatherapy, by Scott Cunningham
I am reading book called Mind Magic by Dr James R. Doty. It is such an empowering book which helps us to understand the science behind the power of manifestation by examining our mindset. He delves...
Read More
December 05, 2024
2025 Webinars, Masterclasses & Events
I'm so excited to share the exciting lineup of masterclasses and webinars for 2025.
With global mental health challenges on the rise, aromatherapy has never been more crucial. I'm passionate about ...
Read More
November 20, 2024
Sal’s 2024 Word of the year and essential oil of the year
The Collin’s Dictionary has chosen ‘brat’ as their word of the year. The word is characterized by a confident, independent attitude. While the word may have traditionally referred to a misbehaving ...
Read More
Book Reviews
October 25, 2024
Dark Nights of the Soul – a guide to finding your way through life’s ordeals, By Thomas Moore.
I discovered Thomas Moore in the midst of the pandemic lockdowns. I found his books profoundly inspiring and compassionate. Dark Nights of the Soul and his highly acclaimed best seller Care of the ...
Read More

Blending Tips
August 27, 2024
The Scent of a Unicorn
The unicorn is a symbol of purity, magic, innocence and power. The unicorn is the most magical of all the mythical animals. The unicorn is often depicted as a pristine white creature, representing...
Read More

Essential Oils
April 26, 2024
My 2023 Word and Essential Oil of the Year
My word of the year is ‘transilience’, a trait we all need, in order to navigate these uncertain and volatile times. There is no need to remind you of the ever-growing list of uncertainties such as...
Read More

Aromatherapy
April 26, 2024
Aromatherapy – bridging lifestyle medicine and functional medicine
I have been asked to speak to a group of undergraduate doctors in their final year of study about aromatherapy. I am both ecstatic and honoured to share my passion for aromatherapy with a group of ...
Read More

Aromatherapy
April 26, 2024
The 2022 Essential Oil of the Year
I was reading about permaculture so that I could improve my gardening skills, so I was therefore excited to see a Guardian article announcing that the word of the year was ‘permacrisis’. What immed...
Read More
Aromatherapy
April 26, 2024
The Wounded Healer and Aromatherapy
The wounded healer archetype has its origins in Greek mythology and shamanic traditions. Images of the wounded healer permeate religion, philosophy, and art and are now used in psychotherapy, couns...
Read More

Health & Wellbeing
April 26, 2024
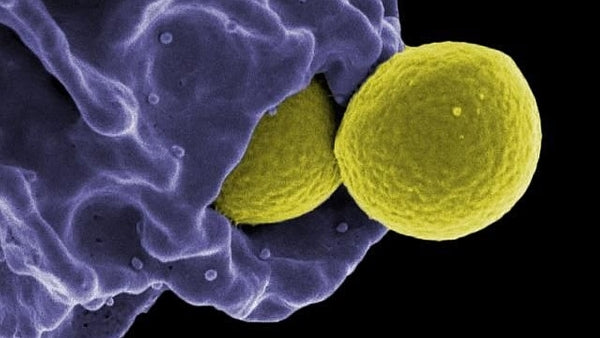
Boosting the Immune System?
The complexity of the immune system is considered secondary only to that of the nervous system.The immune system is classified in two broad categories. The innate immune system (non-specific immune...
Read More
Essential Oils
April 26, 2024
Terrain or Germ Theory?
In the chapter on immunity in the second edition of The Complete Guide to Aromatherapy, I introduced the important role of microbes.1
Read More
Education
April 26, 2024
My upcoming webinars on ways to support the immune system
In Chapter 32 – The Immune System of the second edition of The Complete Guide to Aromatherapy, I introduced the role of microbes by quoting Simon Mills, internationally acclaimed herbal medicine pr...
Read More

Essential Oils
April 26, 2024
Indian Sandalwood Oil in Skincare
In traditional aromatherapy, Indian sandalwood, Santalum album, is commonly used in skincare for dry and sensitive skin. The oil is soothing and cooling, and reputed to have anti-inflammatory activ...
Read More

Essential Oils
April 26, 2024
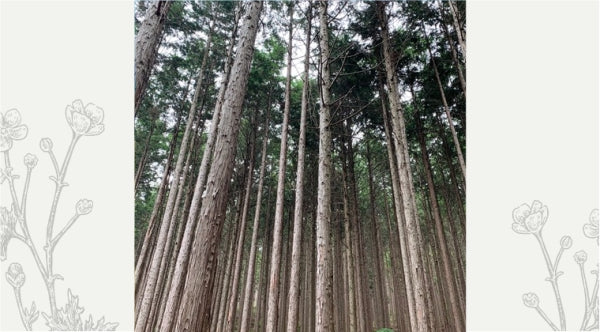
Shinrin-yoku Interviews in Japan
For my Aromatherapy & Shinrin-yoku Webinar, I had originally intended to go to Japan to take you on a tour of the distillery producing our Japanese pure essential oils.
Unfortunately, I was no...
Read More

Essential Oils
April 26, 2024
Aromatherapy and shinrin-yoku
What is shinrin-yoku?
Many cultures have long been aware of the unique relationship we have with nature.
In Japanese, shinrin-yoku is defined as ‘forest bathing’ or ‘taking in the forest atmosphere
Read More

Safety
April 26, 2024
Can I diffuse essential oils around cats?
Several years ago, I wrote a blog to dispel the concern that it is not safe to diffuse essential oils around cats. I did -and still- err on the cautious side by recommending that it is not a good i...
Read More

Essential Oils
April 26, 2024
Are essential oils sustainable?
Personally, I think it is unfair that she has singled out ‘aromatherapy’ and those businesses associated with ‘new age’ movement, as her criticisms are relevant to so many corporations that are inv...
Read More

Essential Oils
April 26, 2024
How Australia is creating a long-term sustainable future for one of the world’s most precious essential oils - sandalwood.
Excessive harvesting of sandalwood trees from the wild without a strategy for replanting has substantially reduced the availability of sandalwood in India. This has resulted in global shortages and...
Read More

Aromatherapy
April 26, 2024
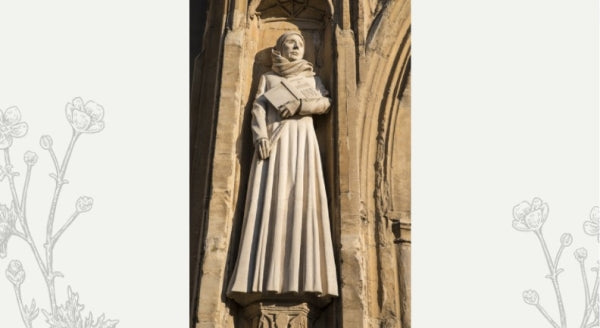
All Will Be Well - The Wisdom of Julian of Norwich and Aromatherapy
The 8th March was International Women’s Day (IWD) and this year’s campaign theme was #BreakTheBias.The official IWD website states that whether deliberate or unconscious, bias makes it difficult fo...
Read More
Essential Oils
April 26, 2024
Don’t worry be happy?
Perfect Potion’s Happy & Calm blend is such a beautiful and simple blend of sweet orange, lavender, Roman chamomile and frankincense. The warm, resiny aroma of frankincense comforts the soul an...
Read More
Health & Wellbeing
April 26, 2024
COVID-19, Aromatherapy and Anosmia – an update
In preparing for my first webinar for 2022, I have referred to the most up-to-date research – which is constantly being updated and revealing the true nature of COVID-19 related anosmia. Much of wh...
Read More

Essential Oils
April 26, 2024
Essential Oils to Flourish
I recently came across a very interesting paper exploring how stress and depression impair the immune system. Furthermore, the study found that emotional stress can weaken the body’s ability to dev...
Read More

General
April 26, 2024
Resilience
This morning I came across a beautiful heartfelt article in the Guardian by Chibundu Onuzo reflecting on the last two years of the pandemic, and how she has come to appreciate the character trait ...
Read More
General
April 26, 2024
Julian of Norwich
In the midst of the long-extended lockdowns that we were experiencing in most places in Australia, I did an online search which involved the words - pandemics, mental health and spirituality. At th...
Read More
Education
April 26, 2024
Essential oil of the year
Many of us have had to deal with the ongoing challenges of the COVID-19 pandemic; associated with COVID infections, lockdowns, travel restrictions and disruption to our normal life. I was hoping th...
Read More
Education
April 26, 2024
My 2022 Free Aromatherapy Webinars
I am so excited to announce the topics and the dates for my 2022 webinars. These webinars will go for approximately 45 minutes and will be free of charge. Please click the links for each webinar fo...
Read More
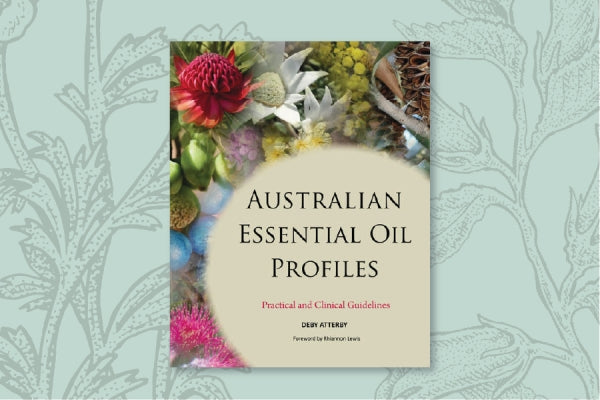
Book Reviews
April 26, 2024
Australian Essential Oil Profiles
By Deby AtterbyPublished: 2021Pages 359
Australia is blessed to be home to a diverse range of aromatic plants, from which some unique and very potent essential oils are produced.
In 2000 I was so ...
Read More
Health & Wellbeing
April 26, 2024
COVID-19 and Anosmia
A recent study reported that one in five people who experienced smell loss as a result of COVID-19 reported that their sense of smell had not returned to normal eight weeks after falling ill. The r...
Read More

General
April 26, 2024
To Flourish
I have always been passionate about aromatherapy as it allows me to flourish; however, what does it mean to flourish?For example, this year we have just established an aromatic garden and it is so ...
Read More
Book Reviews
April 26, 2024
The Empowerment Cycle
Aromatherapist, educator and author Sharon Wood has done an amazing job continuing the legacy she began many years ago when she created Emgoddess.
Read More
Education
April 26, 2024
Aromatherapy & Mindfulness. Interview with Matsuyama-san
In preparing for my Aromatherapy and Mindfulness Masterclass earlier this year, I had the honour and privilege of interviewing highly-esteemed Rev. Daiko Matsuyama: deputy head priest at Taizo-in...
Read More

Health & Wellbeing
April 26, 2024
The role of the gut microbiota and immune responses to vaccination
A 2021 report published in Nature Reviews examines the role of the gut microbiota in modulating immune responses to vaccination
Read More

Health & Wellbeing
April 26, 2024
The Pandemic, Fear, Hope and Resilience
In preparing for my next masterclass, Aromatherapy and Mental Health, I began researching the impact of the pandemic on mental health. The impact of the COVID-19 pandemic on mental health has been ...
Read More

Essential Oils
April 26, 2024
World Gratitude Day
Today is World Gratitude Day. It is wonderful that a day has been dedicated to gratitude. Today, and I hope every day, we can find reasons to express our gratitude. Researchers have now identified ...
Read More

Health & Wellbeing
April 26, 2024
Plant-based diets, pescatarian diets and the severity of COVID-19 symptoms
While several studies have indicated that healthy dietary patterns may play a role in improving the immune response, this was the first study to examine the association between dietary patterns and...
Read More

Aromatherapy
April 26, 2024
Art of Blending Masterclass
Somehow, I knew I was destined to be involved in a life involving scent. Ever since I was a young child I would often sneak into my parent’s room and privately indulge in my mum’s alluring collecti...
Read More

Health & Wellbeing
April 26, 2024
I just had my second jab
I need to start this blog by disclosing that I have just received my second AstraZeneca jab, and to be honest, I am now feeling very relieved. I hope that as more vaccines become readily available ...
Read More
Health & Wellbeing
April 26, 2024
Our role as holistic therapists during the pandemic
The editorial of the Winter 2021 edition of The Australian Journal of Herbal and Naturopathic Medicine by Susan Arentz states that, like other health professionals, naturopaths and herbalists are i...
Read More

General
April 26, 2024
Mother Earth – creating harmony with nature
The concept of biophilia suggests humankind is shaped both cognitively and emotionally through the interactions with nature. However, the prevailing view held by many Western societies is that huma...
Read More
Subtle Aromatherapy
April 26, 2024
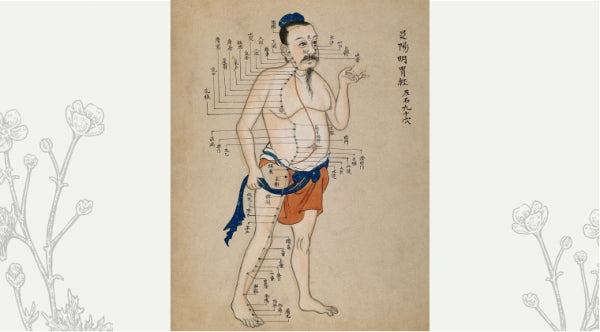
Psyche & Subtle PART FOUR: Biofield Therapies and TCM
In the second edition the title was Subtle Therapies. The change to Biofield Therapies has disappointed several individuals, so please allow me to explain why I decided to change the title of the ...
Read More
Subtle Aromatherapy
April 26, 2024
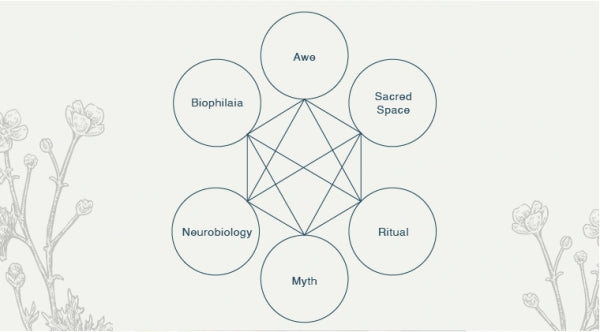
Psyche & Subtle PART THREE: The Spiritual Dimension of Scent
Today we explore Chapter four - the spiritual dimension of scent of my new Volume III of The Complete Guide to Aromatherapy.
Many aromatherapists acknowledge the effect of scent on our psyche. W...
Read More

Subtle Aromatherapy
April 26, 2024
The Psyche & Subtle PART TWO: Sacred Scents
At the 2018 NAHA conference I spoke of The role of scent in culture and spiritual practices, and how this has helped establish a framework for the practice of aromatherapy. In preparing for this p...
Read More
